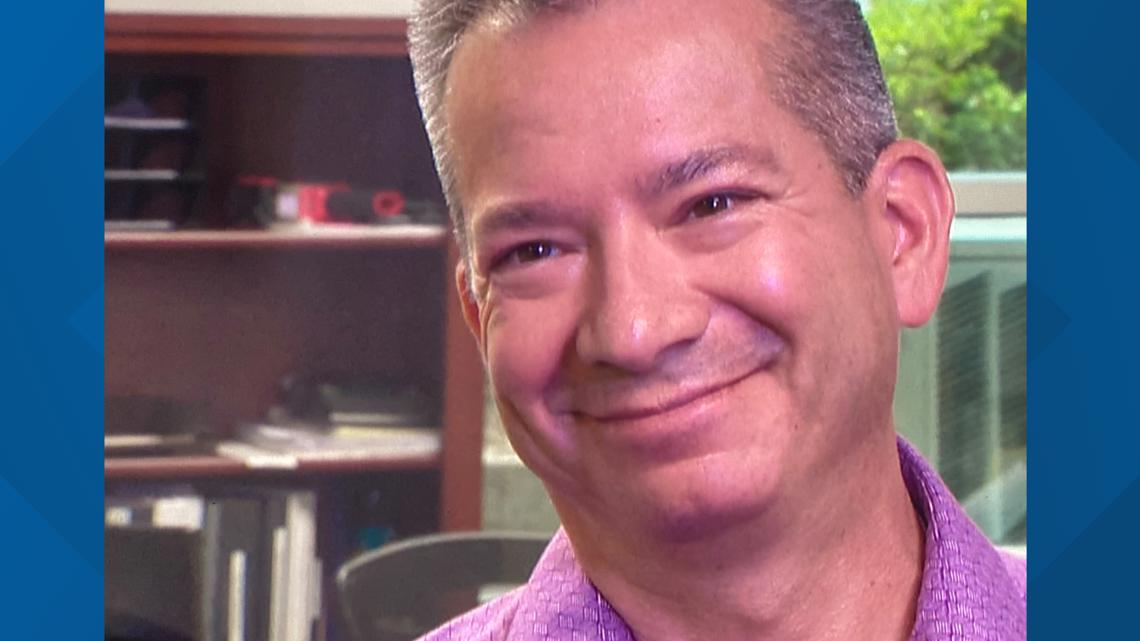
CONCORD, N.C. — The headline of Corey Peña's July 9 email to WCNC Charlotte screamed of desperation.
Closing our doors soon
The content of the email confirmed his heartbreaking situation.
"It’s Corey Peña from Royal Orthotics. Because of nonpayment for our services from managed Medicaid (we) are going out of business. We have borrowed money to keep things going but we are at our end. We will have to sell our home to clear our debt. Know any good bankruptcy attorneys?"
Peña owns a pediatric bracing office in Concord that helps kids walk and be more functional. Instead of seeing patients, Peña said he now spends most of his time troubleshooting the Medicaid claims process.

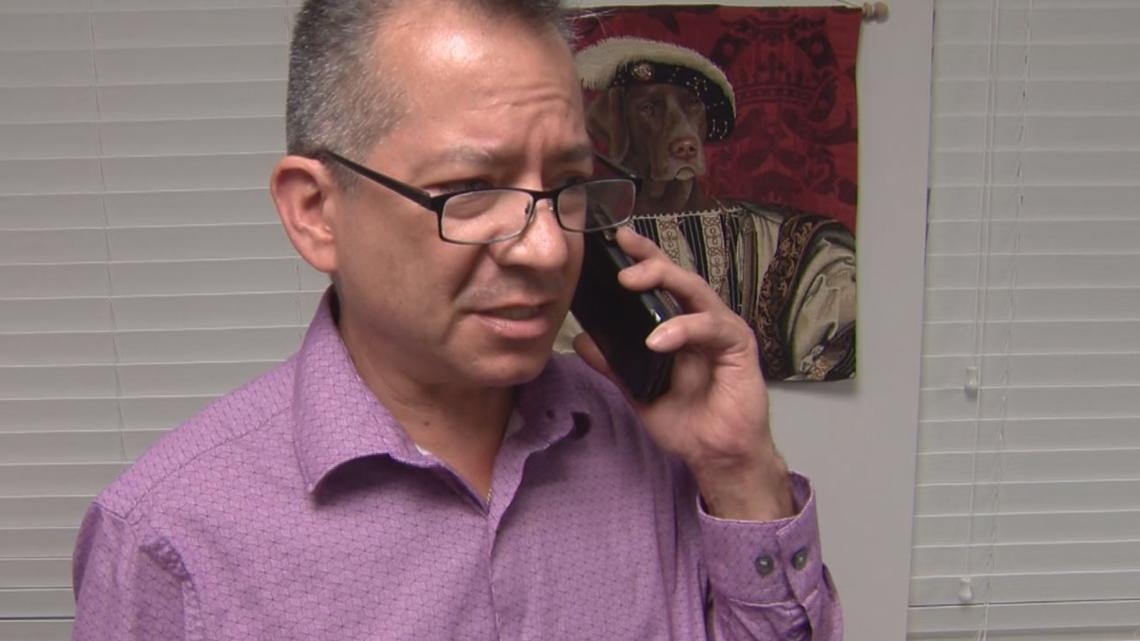
Step inside his empty waiting room and you'll find him expressing his frustration over the phone to one of several prepaid health plans.
"I can't run a business like this. It's unfair and it's unjust," he told one caller. "I'm just beyond words right now."
By July 25, he had documented more than $83,000 in unpaid Medicaid claims that dated back to July 2021. In the meantime, he said his company racked up $144,000 in debt.
"After a year of doing this on my own, I'm like, 'God help me. Help me. I need your help,'" he said of his plea.
After begging for help directly from the state of North Carolina and several of the private companies that now manage the state's Medicaid program, he felt sure God was the only one who would really listen.
WCNC Charlotte is always asking "where's the money?" If you need help, reach out to WCNC Charlotte by emailing money@wcnc.com.

"It's kind of like, 'I'm successful, but I'm having to close my business?'" he told WCNC Charlotte as he stood in front of a vacant desk once used by a now laid-off employee. "That's devastating."
North Carolina spent years preparing for its transition to Medicaid Managed Care. The change, which took effect on July 1, 2021, put five private companies in control of Medicaid. The state's goal was to innovate and put "the health of beneficiaries at the forefront," but in the process, the new managed care approval process left some small medical businesses behind.
WCNC Charlotte documented early payment problems with the changeover. While the state eventually corrected those issues, some smaller providers are still waiting to get paid.

"I'd say Corey's probably not the only one," NC Medicaid Deputy Secretary Dave Richard told WCNC Charlotte. "He did everything right and we just did not deliver and that's on me, it's on our team, it's on our health plans and we'll get better at doing this."
Richard said the program, overall, is serving the needs of low-income and vulnerable patients and largely reimbursing medical providers in a timely fashion, but he conceded there's room for improvement.

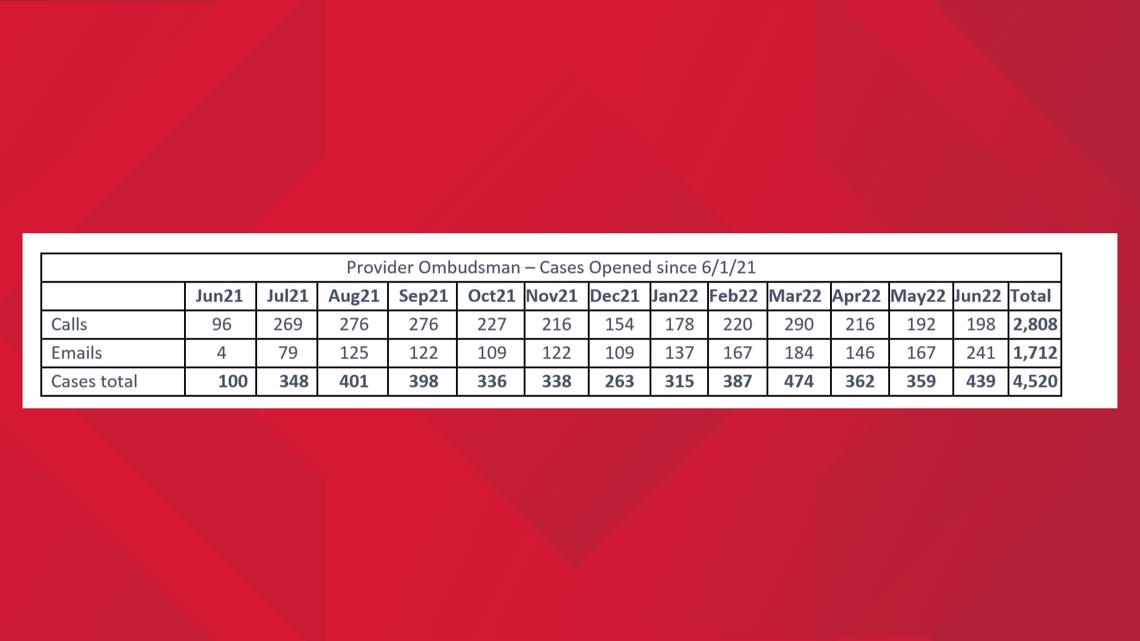
State data show the NCDHHS Division of Health Benefits’ Provider Ombudsman has received an especially high number of complaints in recent months. More than a third of those complaints are tied to claims and reimbursements, according to state records.
Richard said the state is digging deeper into the data to identify the reason behind the rise in complaints but believes they're tied to timely filing deadlines.
"The numbers that we're seeing, although concerning, they're very small numbers still at the Ombudsman level," Richard said, citing the more than 30 million claims paid out over the last year. "We've seen some places where we have to do better with our providers."
One of those areas, he said, is claim approval. State data revealed the five companies running the program are denying a little more than one out of every four claims.
"I think we're seeing a higher denial rate than we want," Richard said. "What we want to have happen is that every claim that is a legitimate claim, gets paid and it gets paid as soon as possible."
As an extra incentive, the state has penalized the health plans when they don't live up to their ends of the bargain. Medicaid records show the five companies that now manage Medicaid have paid just under $1 million, combined, in fines.

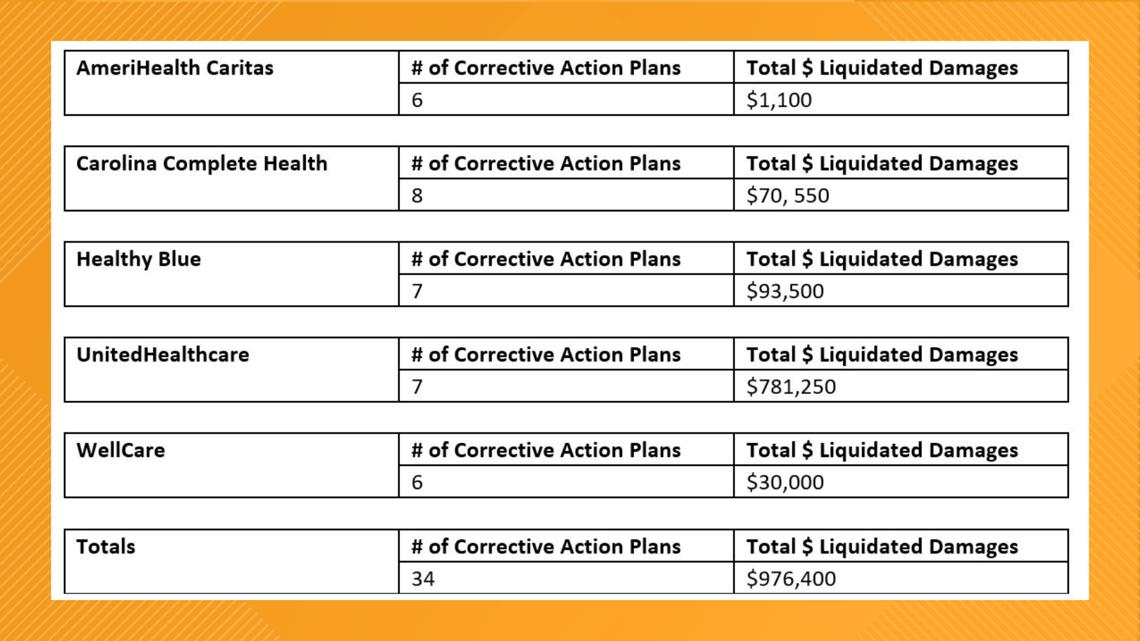
"If you have to pay a financial penalty, it's probably a thing that gets people's attention most quickly," Richard said.
Despite the fines and complaints, the North Carolina Association of Health Plans maintains the Medicaid transition has been among the "smoothest in the nation."
"We are now 12 months into the launch of Medicaid Transformation. We are pleased to share that the launch of North Carolina's program has been among the most comprehensive and yet smoothest in the nation," Executive Director Peter T. Daniel said in a statement to WCNC Charlotte. "Having said that, health plans are working diligently to address individual provider issues and identify solutions. In response, the health plans take a 'no wrong door' approach when responding to provider inquiries. As a result, we are proud to report, across all health plans, that a clean claim is paid on average within 11 days. As North Carolina's program matures, we are excited about the opportunity to build on the hard work of the North Carolina Department of Health and Human Services and our provider partners to complete a successful transition to Medicaid managed care."
The deputy secretary said he's made it clear to those companies they need to focus on getting it right for smaller providers like Peña.
"We hate what happened to this one provider. We think, in general, the program is going well. We think it will continue to improve, but we can't have providers put in this situation and we will work every day to make sure we resolve that," Richard said.
For Peña, action has taken far too long. WCNC Charlotte first amplified his problems in November.


"I wasn't ready for a year of hearing, 'Oh, we'll fix it. Oh, we'll take care of it,'" he said. "Why was this allowed to happen?"
At the time, WCNC Charlotte shared details of the scope of his unpaid claims with NC Medicaid.
"There's no excuse for this," Richard said. "We thought it had been corrected. My fault for not digging deeper to make sure it had been."
Richard and Peña have communicated directly in recent days. The small business owner has also received help from a state lawmaker and assurances from some of the Prepaid Health Plans.

If a text message to WCNC Charlotte Thursday is any indication, Peña is about to get paid. The small business owner detailed a "good and productive" three-hour meeting with representatives of one of the PHPs, including the company's CEO, who promised a $37,000 check in the coming days.
"This is a miracle of God," Peña said full of hope. "I believe and trust that this situation is going to turn around. It hasn't happened quite yet, but I'm not selling my house."
Contact Nate Morabito at nmorabito@wcnc.com and follow him on Facebook, Twitter and Instagram.
WCNC Charlotte is committed to reporting on the issues facing the communities we serve. We tell the stories of people working to solve persistent social problems. We examine how problems can be solved or addressed to improve the quality of life and make a positive difference. WCNC Charlotte is seeking solutions for you. Send your tips or questions to newstips@wcnc.com.

