Nursing homes fined for poor infection control received federal COVID-19 bonuses
A WCNC Charlotte investigation identified more than 100 nursing homes in the Carolinas that received incentive payments despite paying fines for violations.

A WCNC Charlotte investigation revealed nursing homes that were fined thousands of dollars after deadly COVID-19 infections spread within their walls also collected government bonuses that, in most cases, offset their original penalties.
WCNC Charlotte's analysis of two sets of federal data identified more than 100 nursing homes in the Carolinas that collected federal incentive payments despite infection control and COVID-19-related penalties, receiving a combined $10 million more in bonuses than penalties.
More than 80% of those nursing homes also had at least one resident die from COVID-19 since March 2020, according to an analysis of Pro Publica's Nursing Home Inspect database.
WHO GOT PAID: Use this database search tool to search for a city or a nursing home to see which ones received federal incentive payments
'It's totally sickening'
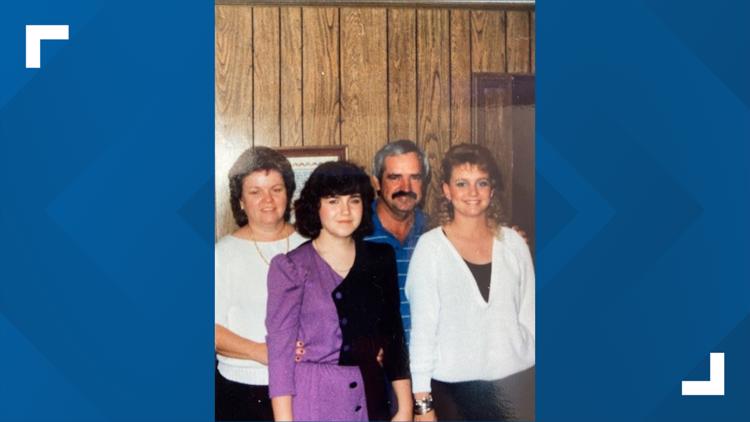
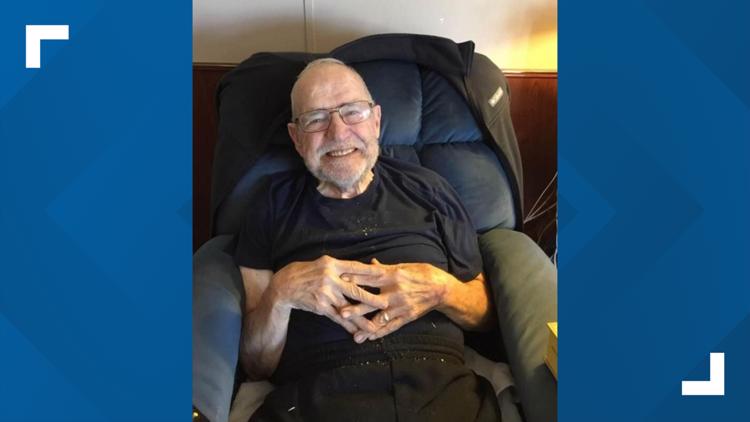
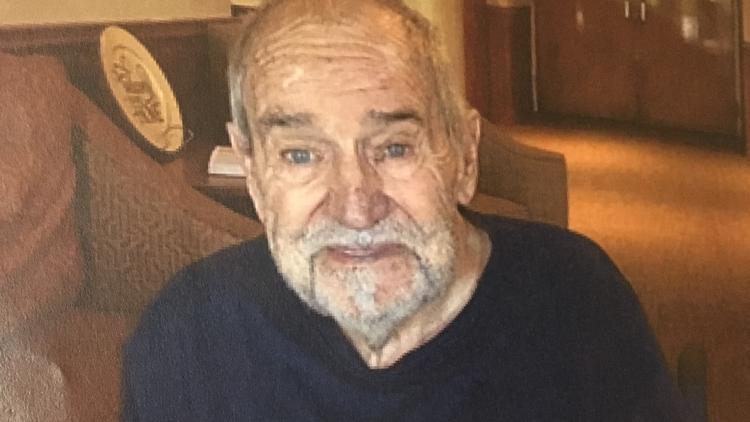
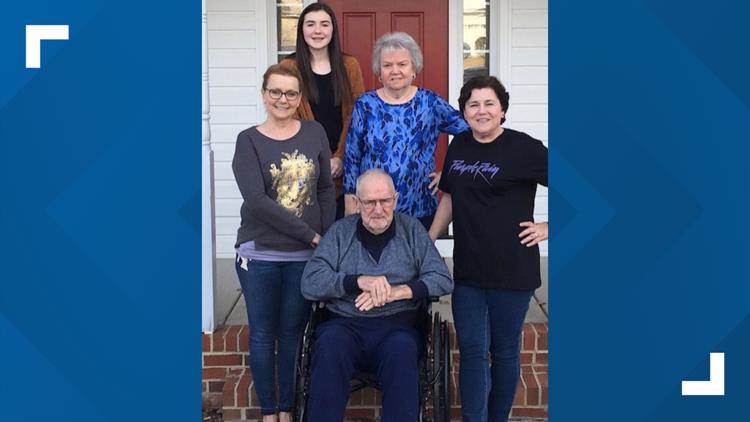
Kelly Moody Fesperman and her sister Lisa Dawn Moody couldn't stop shaking their heads when WCNC Charlotte shared the discovery. Their 78-year-old father, Kenneth Moody, died from COVID-19 in April 2020, just three weeks after entering The Citadel Salisbury.
"It's hard to even imagine," Fesperman said. "It's so shocking. It's like you're numb when you hear that."
Following inspections in 2020, the Centers for Medicare and Medicaid Services, an agency within the U.S. Department of Health and Human Services, fined The Citadel Salisbury a combined $359,000, according to government records.
In a May 2020 report, inspectors cited a "system failure" that likely placed residents at an increased risk of COVID-19, concluding the nursing home failed to quarantine some new residents, failed to quickly follow CDC face mask guidance, didn't promptly notify residents and/or their families of positive test results and even neglected to notify one family of a loved one's death.
Kenneth Moody is listed as Resident No. 11 in that report, according to the family's attorney. Inspectors found The Citadel failed to place Resident No. 11 in quarantine when he first arrived. Instead, the facility gave him a roommate, according to the report. Inspectors also cited his missing mask when his family visited him through windows in the lobby.
"We were told he would be in a private room for two weeks, sort of like a quarantine, so we assumed that would happen," Moody said. "It didn't happen. He was put into a room with a roommate. After he passed away, we found out the roommate had COVID."
Moody died on April 21. His daughters said they had to say goodbye over FaceTime.
"[The doctor] said, 'Your dad is dying,' and we didn't even know he was sick," Fesperman said.
Kenneth Moody through the years
"I don't want any other family to go through what we've had to go through," Moody said.
Rowan County records show 18 people died from COVID-19 at The Citadel Salisbury. In all, the country reports 189 cases of illness there.
While Moody's daughters and other families grieved, federal records show the Health Resources and Services Administration, another agency within the U.S. Department of Health and Human Services, awarded The Citadel Salisbury $194,000 unsolicited for reducing COVID-19 infection rates relative to their county and mortality rates against a national benchmark in October and December of 2020.
WCNC Charlotte is always asking "where's the money?" If you need help, reach out to the Defenders team by emailing money@wcnc.com.
"It just makes me sick," Fesperman said after hearing that finding. "It's totally sickening."
Moody shared a similar sentiment.
"Angry and sad that people are still there," Moody replied.
The HRSA defended the incentive payments, citing the fact that the pandemic has disproportionately impacted nursing homes. According to the federal agency, every nursing home that received payments through the new program was checked to make sure they had active, non-terminated certifications and were checked against National Healthcare Safety Network quality checks.
Recipients must also comply with strict rules in using the money to protect residents and staff against COVID-19 with the risk of recoupment for any found to be in non-compliance, according to HRSA.
Nursing homes win, residents lose
Brian Lee runs the national nursing home watchdog group Families for Better Care. He calls what played out with federal money inside the U.S. Department of Health and Human Services a best-case scenario for nursing homes.
"I think this is about the saddest commentary of this pandemic when it comes to our nursing homes," Lee said. "Unfortunately, the nursing homes, as they normally do, they win and the residents lose."
For years, Lee served as Florida's long-term care ombudsman.
"In too many of those cases, the feds have given back the money to [these nursing homes] in bonus payments, so it offsets the enforcement," Lee said. "It waters down the oversight, the accountability. It is an erosion of enforcement. It is an erosion of accountability. It sends a message that our loved ones' lives just didn't matter."
Some in the industry aren't convinced either the incentives or the penalties made sense during the pandemic. The American Health Care Association went so far as calling for a major overhaul earlier this year, saying the current oversight system is too "focused on a punitive approach rather than improvement."
The North Carolina Health Care Facilities Association, meanwhile, supports the incentive payments.
"Throughout the pandemic, North Carolina nursing homes have worked tirelessly under incredibly challenging conditions to care for our state's most vulnerable citizens," CEO Adam Sholar said in a statement. "The incentive program, which provided payments to many facilities across the country with better patient outcomes near the end of the year, [was] part of the federal government's overall array of support for healthcare providers during a particularly challenging period of the COVID-19 pandemic. These payments, like other support from the Provider Relief Fund, enabled these facilities to invest in their staff and further improve patient care."
Which got paid?
Provider Relief Fund COVID-19 Nursing Home Quality Incentive Program records show more than 550 nursing homes in the Carolinas received at least one incentive payment for their performance in September, October, November and/or December.
WCNC Charlotte is always asking "where's the money?" If you need help, reach out to the Defenders team by emailing money@wcnc.com.
Federal records show, in addition to The Citadel Salisbury, inspectors fined more than a dozen of Accordius Heath's other nursing homes. Those facilities also benefited from the incentive program, according to federal data.
The company, through a spokesperson, declined comment for this story.
Class-action lawsuit
Attorneys filed a class-action lawsuit against The Citadel Salisbury, Accordius Health and the company's owners Monday, alleging understaffing and poor resident care.
"Our firm is proud to represent families who have had many loved ones at The Citadel Salisbury and other Accordius Health facilities," attorney Mona Wallace said in a statement. "Our clients remain very concerned about the conditions at these nursing homes and the lack of transparency by the corporations that control them. They are also concerned that government efforts to regulate the industry do not go far enough. We are hopeful that continued public discussion of the issues will lead to positive change in the nursing home industry."
Kenneth Moody's daughters have since put their trust in that law firm.
"These are human beings that have life stories that have people that love and care for them," Fesperman said.
"I feel sorry for the ones that are left there," Moody said.
How to research a nursing home
When it comes time to choose a nursing home for your loved one, the decision can feel overwhelming.
Lee said it's critical people do their research before placing their loved one in a nursing home. Families for Better Care lists four tips:
1. Check the facility ratings on Nursing Home Compare's website
Nursing homes are inspected every 9 to 15 months or whenever a complaint is lodged with the state's regulatory agency. These reports are available online along with a star rating for each facility.
Facilities rated with a 1-star or 2-star ranking denote frequent and/or serious problems whereas 4-star or 5-star homes denote better-operating facilities.
Compile a list of facilities that have a good record and move on to step two.
2. Call your local ombudsman office and ask for additional information
The Long-Term Care Ombudsman is a federal and state-mandated advocacy program. Ombudsmen regularly visit residents and investigate complaints from a resident's perspective.
The Ombudsman Program is a treasure trove of information. Program staff and volunteers are very knowledgeable about laws and regulations that govern resident care. Using your list from step one above, ask the ombudsman office to provide you a summary of complaint data for each facility you identified. Also, ask to speak with the ombudsman who visits the facility as they can give you further insight on resident care.
And if problems ever arise at the nursing home, they will gladly help. The program offers free services and all complaints are confidential.
3. Schedule nursing home tours
(IMPORTANT: Make sure to plan some visits at night or over the weekend, problems typically occur during these shifts)
When you arrive, don't be star-struck by the lobby. Nursing homes invest a great deal of money in their lobbies to make them feel warm and inviting, but this can often be fool's gold. Care happens beyond the administrator's office. Don't be afraid to walk around the facility and ask some tough questions.
Spend considerable time talking with families and residents without staff present. They'll give you an honest assessment of what life is really like in the facility.
Watch out for these red flags, they are frequent indicators of negligent or abuse care:
- Not enough staff to promptly respond to resident calls for assistance
- The facility smells of urine, feces or chemicals
- Food does not look or taste appetizing
- Residents are left unattended for long periods of time
- Residents appear disheveled or are wearing mismatched/stained clothes
- Dead bugs or rodent droppings sprinkled throughout the resident living areas
- Furniture is in disrepair, floors are sticky
- Staff are impolite or disrespectful
- Staff fail to knock before entering residents' rooms
- Too few or no activities (check to see if current activities match what's posted in the activity calendar)
- No resident or family council
4. Make a decision
Following these steps should give you enough information to avoid a nursing home placement misstep.
If the need for nursing home care is suddenly thrust upon you, call your local ombudsman immediately. Program staff have nursing home information readily available and can help you make an informed, albeit quick, decision.
Contact Nate Morabito at nmorabito@wcnc.com and follow him on Facebook, Twitter and Instagram.