RICHLAND COUNTY, S.C. — Throughout the pandemic nurses have been called our ‘healthcare heroes,’ but, like many others, the emotional toll for them has been steep.
“It was always that fear that will I get it, and that is not a good feeling,” Dr. Kim Gilmore, a roughly 35-year nurse, said. “You try not to think about it because you’re doing a job and you’re being compassionate and trying to help others, but it does cross your mind all the time.”
From her Richland County office, Dr. Gilmore helps patients cope with their mental and behavioral needs, but said she too, at times, has coped with anxiety and sadness, especially when learning of colleagues who have died from virus-related complications.
“I mean, I became dazed,” Dr. Gilmore said. “I’m not even on the front lines seeing all these people dying. How does this really impact the nurses that are on the front lines, you know with the multiple deaths every day?”
Dr. Gilmore, who also chairs the State Nursing Association’s Psychiatric-Mental Health Chapter, said she wanted other nurses to know they’re not alone.
“This pandemic has wreaked havoc on our nurses emotionally,” Felicia Heyward, a psychiatric mental health specialist, said. “The physical stressors from working these extra-long shifts and having to be somewhat detached for the norms of our patient care. We’re wearing PPE. We’re not able to do those hugs that we normally do to make patients feel better, and I think, just everything in general. The unknown is the biggest, probably some of the biggest stressors that we’ve been seeing.”

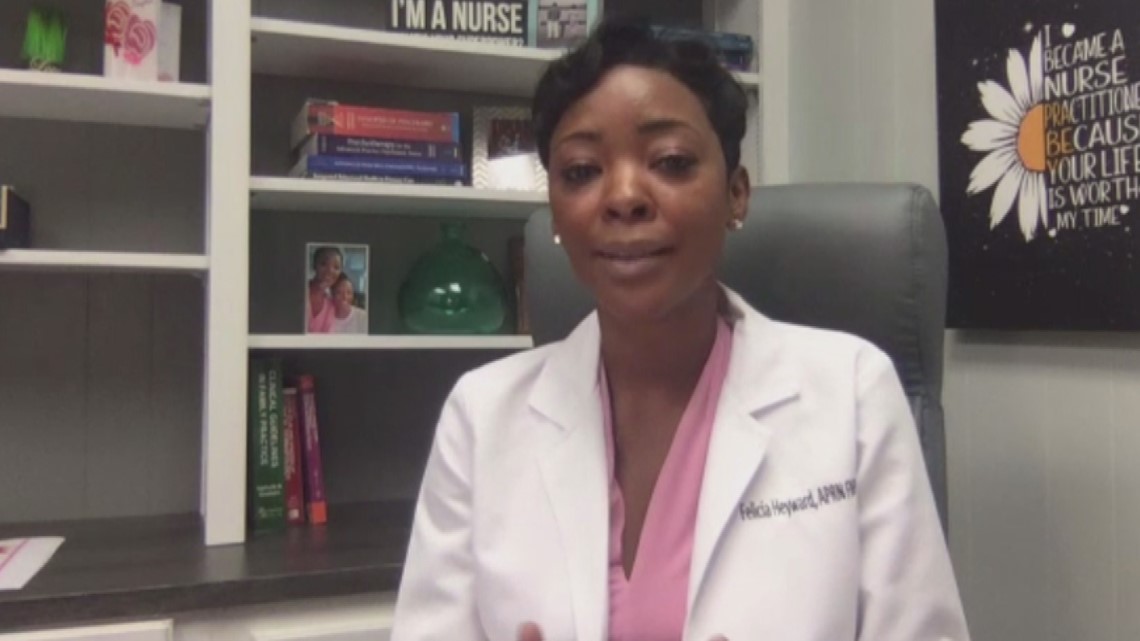
While nurses often feel compelled to help, Heyward, who is also a family nurse practitioner, said it’s okay to ask for a helping hand with resources often available through employers.
“My biggest message for our nurses is to understand that it’s okay to not be okay and that you’re not alone in the struggles that you are facing emotionally,” Heyward said. “Mental health counseling is a great tool for nurses to be able to speak freely and just be aware of their own mental wellness and be able to rebalance and get back to a normal state of mind.”
For Gilmore, knowing the vaccines are more available along with talking out her feelings, she said, have helped. Now, she just wants others to know it’s okay to ask for assistance.
“Sometimes the provider does need a provider and it’s okay,” Dr. Gilmore said. “We can’t be strong all the time.”
Whether you’re a nurse or just someone facing a challenging time, there are resources available.
Heyward recommends reaching out to your family health care provider or seeking counseling services for assistance. Resources are also available at CDC.gov.

