The wrong diagnosis: What happens when doctors are wrong?
<p>At only 37 days old, Heather's newborn was acting strange — screaming, her arm hanging limp.</p>

At only 37 days old, Heather's newborn was acting strange — screaming, her arm hanging limp.
It was a scary scenario, especially for a new mother. So Heather took baby Autumn to the hospital.
"They did an x-ray on her arm,” Heather said. “They came back and said it was broken. We were in shock."
Autumn's arm wasn't just broken, it had 21 fractures. The doctor claimed those injuries were in places that could've only happened from squeezing and physically abusing the child. As protocol, the hospital notified Child Protective Services, who interviewed Heather and her then-boyfriend.


"We had nothing to hide,” Heather said. “So we kept trying to help them figure out what happened to my daughter. And after interviewing the two of us, they said they were taking custody of her."
This was in 2010.
Despite her claims of never abusing Autumn, Heather and her then-boyfriend, non-biologically related to her daughter, were charged criminally. She spent 60 days in jail. He served two and a half years.
In the meantime, Autumn was placed in the custody of her biological father.
"It's extremely frustrating,” Heather said. “You have no answers, you have no idea what's going on. It's a completely foreign situation and your child is gone. It's completely devastating and if you don't have the resources to fight like money or if you're not very well-educated or maybe you speak a different language, it's terrifying."
But Heather decided to hire an attorney, who took all of Heather and Autumn's documents — OBGYN records, medical papers, baby well care documents — and decided to get a second opinion on the doctor's diagnosis.
That attorney found a doctor who said the original diagnosis was wrong. That this wasn't a case of child abuse. He wrote a report stating Autumn suffered from a metabolic bone disease called Rickets, which causes softening and weakening of the bones.


Heather's attorney got nearly a dozen other experts to testify that this was a misdiagnosis.
Finally, Heather was able to get shared custody of Autumn with the biological father. But that took almost seven years.
"I missed all of her firsts, you know,” Heather said. “And all you can do is send packages to whoever may have your child, care packages or whatever they may need. That's the only parenting you get really.”
According to Dr. Michael Laposata, chairman of the pathology department at the University of Texas, misdiagnoses of patients happen more often than we think.
"I have been presented with a lot of children who have bruises. And many of the caregivers, in these cases, have been accused of inflicting the bruises on the child," Dr. Laposata said.
He also says every adult American has gone through at least one diagnostic error in their lifetimes. And even though this has been happening for decades, it's really only come to the public's attention in the past two to three years.
Laposata says a diagnostic error happens in one of three ways:
1) The diagnosis is completely incorrect — i.e. the doctor says you have anxiety when you have a heart problem.
(2) The diagnosis is delayed — i.e. the doctor presents the problem a week later, or a month later.
(3) The diagnosis is not explained properly to the patient.
Laposata says the United States spends $2.2 trillion in health care, however, $800 billion of that is wasted. And it's not that doctors don't care about their patients, rather, they're human.
Laposata says it's nearly impossible for any one medical expert to know everything there is to know. So what is the solution to reducing misdiagnoses? Laposata said diagnostic management teams.
He added that doctors need to coordinate with nurses, radiologists, oncologists, and everyone else. They need to constantly be speaking with other medical experts related to the case, rather than relying solely on one opinion.
The UC Davis Medical Center already has these management teams in place for the clinical chemistry lab. Research teams work with nurses, clinicians, and therapists to both prevent errors and reverse them. Medical experts from the hospital say they've had a breakthrough with glucose meters.
Glucose meters were once all thought to be the same in all medical facilities. Dr. Nam Tran, director of the clinical chemistry lab at UC Davis Medical Center, said if you give a person more insulin than they need, their glucose levels drop down too low and that can potentially kill them.

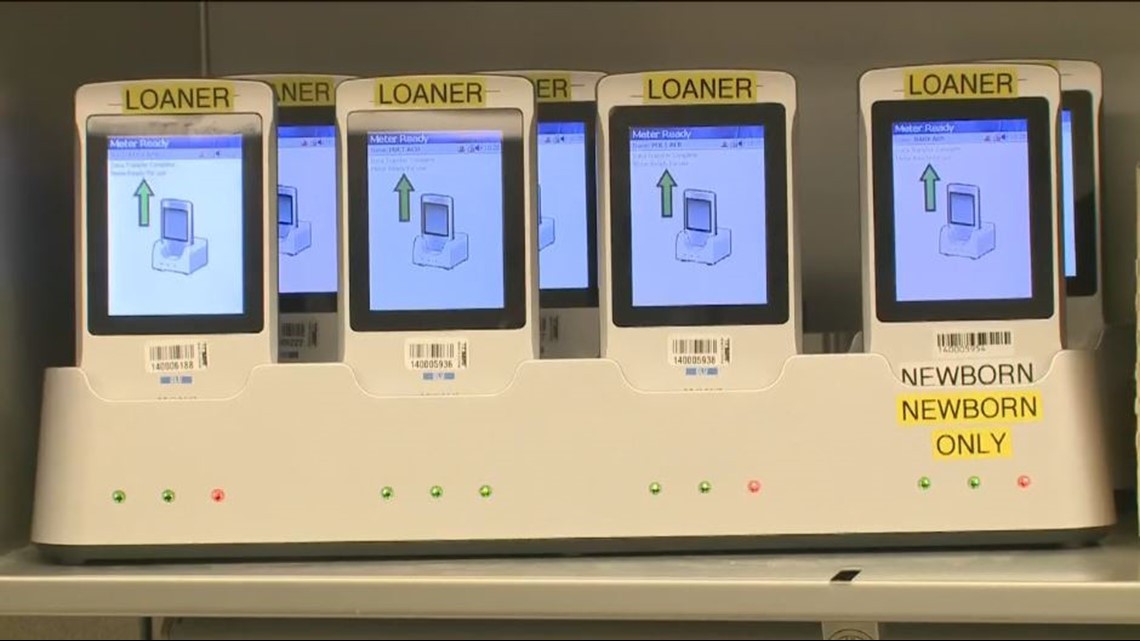
“We test thousands upon thousands of glucose measurements per day, and we give patients a lot of insulin per day,” Tran said. “And if you can minimize erroneous insulin administration, you probably made patients do a lot better in their hospital stay."
Tran says their research, in part, prompted the Food and Drug Administration to enforce better quality glucose meters in 2014 throughout the nation. Even after switching out their own meters at the UC Davis Medical Center, researchers noticed hypoglycemic issues drop by 35 percent in patients.
"There needs to be accountability for these doctors who are making these rash decisions and taking these children," Heather said. Her criminal conviction was finally overturned this year.
In the meantime, Heather helps other families going through similar situations with her Facebook page.